When you start ADHD medication, you’re not just looking for focus-you’re hoping for a better day, better grades, less frustration. But for many, the conversation quickly turns to side effects: heart rate, blood pressure, trouble sleeping. These aren’t just side notes. They’re real, measurable, and often overlooked until they become a problem.
How ADHD Stimulants Work-and Why They Affect Your Heart
ADHD stimulants like Ritalin, Concerta, Adderall, and Vyvanse work by boosting dopamine and norepinephrine in the brain. That’s what helps with attention and impulse control. But these same chemicals also activate your nervous system’s fight-or-flight response. That’s why your heart beats faster, your blood vessels tighten, and your blood pressure rises-even if you’re just sitting at your desk. It’s not dramatic. Most people see a rise of 1-4 mmHg in systolic blood pressure and 1-2 extra beats per minute in heart rate. Sounds small? It is. But over time, even small changes add up. A 2025 study from the University of Southampton, the largest of its kind, looked at data from dozens of clinical trials and confirmed: these changes happen consistently across all major stimulants, whether they’re methylphenidate or amphetamine-based. And it’s not just stimulants. Even non-stimulant medications like atomoxetine and viloxazine show similar effects. That’s a surprise to many doctors who assume only stimulants are the issue. Guanfacine, on the other hand, actually lowers blood pressure and heart rate-making it a rare ADHD medication that might help both focus and cardiovascular health.What Does the Research Say About Long-Term Heart Risks?
The big fear? Sudden cardiac events. In 2006, the FDA issued a warning after 25 cases of sudden death in people taking ADHD meds. That sent shockwaves through the medical world. But here’s what the data now shows: the absolute risk is extremely low. A 2024 JAMA Psychiatry study followed over 14,000 people for 14 years. It found that long-term stimulant use was linked to a 17% higher risk of cardiovascular disease-mainly high blood pressure and artery problems. But that’s not the whole story. The study also showed that the risk increased with higher doses and longer use, especially in the first three years. Still, the actual number of people affected? Very few. The number needed to harm for a serious event is over 1,000. In other words, for every 1,000 people on stimulants, maybe one might have a cardiovascular issue directly tied to the medication. A 2024 study from the American College of Cardiology found that young adults on stimulants were 17% more likely to develop cardiomyopathy (a weakened heart muscle) after one year, and 57% more likely after eight years. But again-absolute risk remains small. The lead author, Dr. Pauline Gerard, put it plainly: “It’s a real risk, but it’s small.” For people with existing heart conditions, the picture changes. Those with Long QT Syndrome-a rare electrical heart rhythm disorder-are at higher risk. Some studies show increased fainting episodes; others show no increased events. The bottom line? If you or your child has a known heart rhythm issue, talk to a cardiologist before starting stimulants. It’s not a hard no, but it’s a hard look.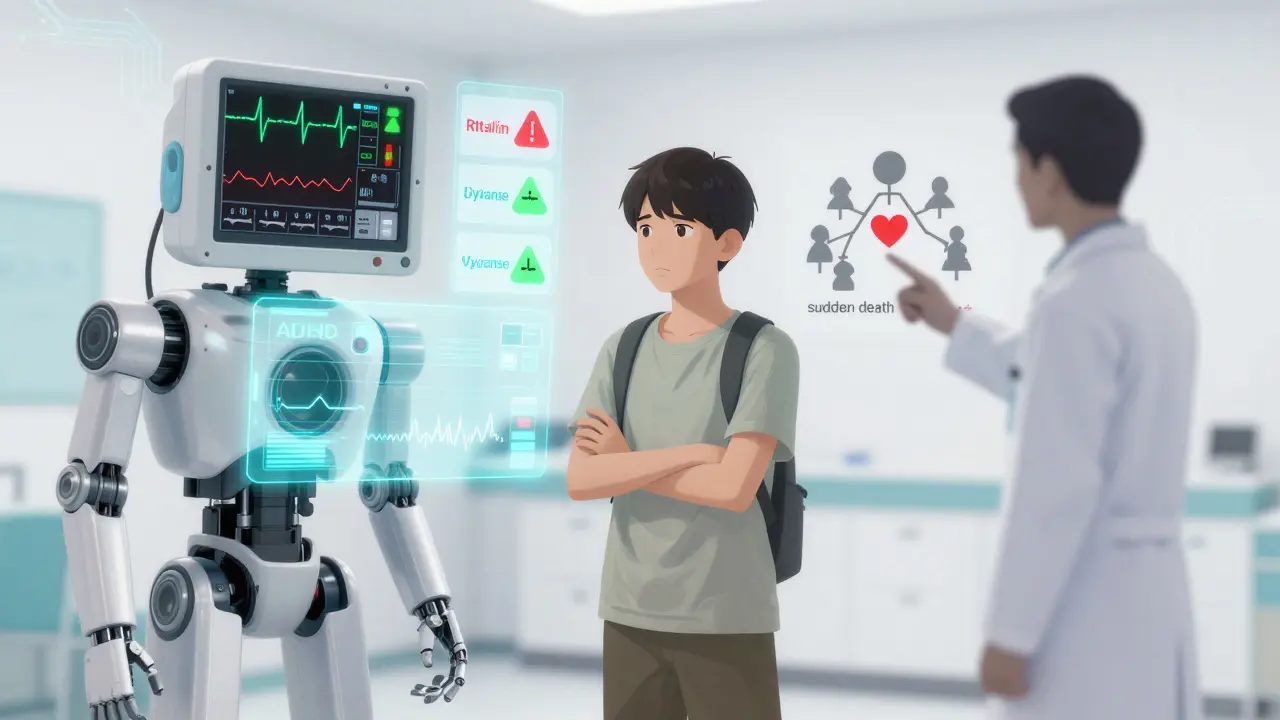
Who Needs Screening? ECGs, Blood Pressure, and Family History
Should everyone get an ECG before starting ADHD meds? The American Heart Association once said yes. Now, they’ve backed off. The American Academy of Pediatrics never supported it. And current guidelines from the American Academy of Neurology say: skip routine ECGs. Instead, the focus is on history. Ask these questions before prescribing:- Has anyone in your family died suddenly before age 40?
- Have you ever passed out during exercise?
- Do you have chest pain, shortness of breath, or palpitations?
- Have you ever been told you have a heart murmur or high blood pressure?
Sleep Problems: The Silent Side Effect
If your child can’t fall asleep, or you’re tossing and turning at 1 a.m. after taking your afternoon Adderall, you’re not alone. Between 30% and 50% of people experience sleep issues when starting stimulants. For some, it’s temporary. For others, it sticks around. Why? Stimulants stay in your system longer than you think. Extended-release versions like Concerta or Mydayis can still be active 10-12 hours after taking them. That means your brain is still buzzing when it’s time to wind down. Studies show stimulant users take 15-30 minutes longer to fall asleep than those on placebo. And while this often improves after a few weeks, it doesn’t disappear. That’s why timing matters. Take your medication as early in the day as possible. If you’re still struggling, talk to your doctor about switching to a shorter-acting form or reducing the afternoon dose. Melatonin-0.5 to 5 mg, taken 1-2 hours before bed-can help reset your sleep clock. It’s not a magic fix, but it’s safe and often effective. For people who can’t tolerate sleep disruption, non-stimulant options like atomoxetine or guanfacine are worth considering. Guanfacine, in particular, has been shown to improve sleep quality in some patients, even while helping with focus.
