Imagine you’re in the hospital, unable to speak. Your heart is failing. Your kidneys are shutting down. The doctors ask: Should we give her the antibiotic? What about the painkiller? Should we stop the blood thinner? Your family is gathered around, but no one knows what you’d want. That’s not a hypothetical. It happens every day. And it doesn’t have to.
What a Medical Power of Attorney Actually Does
A Medical Power of Attorney (also called a Healthcare Proxy or Durable Power of Attorney for Health Care) is a legal document that lets you name someone you trust to make medical decisions for you if you can’t. It doesn’t kick in while you’re awake and able to speak. It only activates when you’re unconscious, severely confused, or otherwise unable to communicate. That’s it.This isn’t about giving up control. It’s about keeping it - even when you can’t speak. The person you choose, your agent, becomes your voice. They don’t make decisions based on what they think is best. They make them based on what you told them you’d want.
And that includes medication. Not just whether to give you antibiotics or pain meds. But which ones. How they’re given. Whether you’d accept a drug with side effects that scare you. Whether you’d refuse a medication that feels like it’s just prolonging suffering.
All 50 states recognize this document. But the rules vary. Some states need two witnesses. Others require notarization. Indiana requires your doctor to sign off if it’s about psychiatric meds. California? Just your signature. You can get free, state-specific forms from LawHelp DC or your state’s health department. No lawyer needed - unless your situation is complex.
Why Medication Decisions Are the Biggest Blind Spot
Most people think advance directives are about ventilators and feeding tubes. Those are important. But the real daily battles happen over pills and injections.A 2023 study in the Journal of Pain and Symptom Management found that patients with a named healthcare proxy had 32% fewer conflicts over medication during hospital stays. Why? Because decisions about pain relief, antibiotics, sedatives, and psychiatric drugs come up constantly - often in moments of crisis. Without clear guidance, families panic. Doctors hesitate. Medications get delayed. Or worse - given when you’d have refused them.
One Reddit user, NurseJen42, shared how her mother’s POA prevented a 12-hour delay in antibiotics during sepsis. The hospital didn’t know her allergies. But her agent did. That’s the power of this document.
But here’s the problem: 41% of agents surveyed by the Conversation Project said they were uncertain about their loved one’s medication preferences. 37% wished they’d known more about painkiller choices. A case in Indiana involved an agent refusing blood thinners because they misunderstood the patient’s wishes - leading to a preventable stroke.
It’s not that people are bad decision-makers. It’s that most never talked about it. They assumed their agent “just knows.” They don’t.
Living Will vs. Medical Power of Attorney: Which One Do You Need?
You’ve probably heard of a living will. It’s a document that says, “If I’m in a coma, don’t keep me alive.” Simple. Clear. But it’s also limited.A living will can’t cover every scenario. What if you get pneumonia and need antibiotics? What if your dementia gets worse and you refuse to take your antidepressants? What if a new drug becomes available that could help - but you’ve never heard of it?
A Medical Power of Attorney fills those gaps. Your agent can look at the situation, talk to the doctors, and decide based on what you’ve told them - not just what’s written on paper.
Think of it this way: A living will is a map with one road marked. A healthcare proxy is someone who knows the whole region, can read the weather, and can choose the best route - even if it’s not on the map.
Most experts agree: You need both. But if you can only do one, pick the Medical Power of Attorney. It’s more flexible. More powerful. More human.
Who Should Be Your Agent? (And Who Shouldn’t)
This isn’t about who’s the oldest, richest, or most responsible. It’s about who knows you best.Choose someone who:
- Has had real conversations with you about your values - not just “I don’t want to be a burden.”
- Can handle stress without crumbling.
- Won’t be swayed by other family members.
- Knows your feelings about medication - especially pain meds, sedatives, and psychiatric drugs.
Avoid choosing:
- Your doctor (it’s a conflict of interest).
- Your primary caregiver if they’re also your heir (some states ban this).
- Someone who disagrees with your beliefs - even if they’re “logical.”
One man in Pennsylvania named his daughter as agent. But she didn’t know he’d refused opioids after his back surgery in 2018 because they made him nauseous. When he got sick again, she agreed to the same drug - because she didn’t know the history. He suffered for days.
It’s not her fault. It’s because they never talked about it.
How to Talk About Medication Preferences - Without Scaring Anyone
Talking about death and drugs is hard. But you don’t need to say, “I don’t want to be kept alive.” You can start small.Try this:
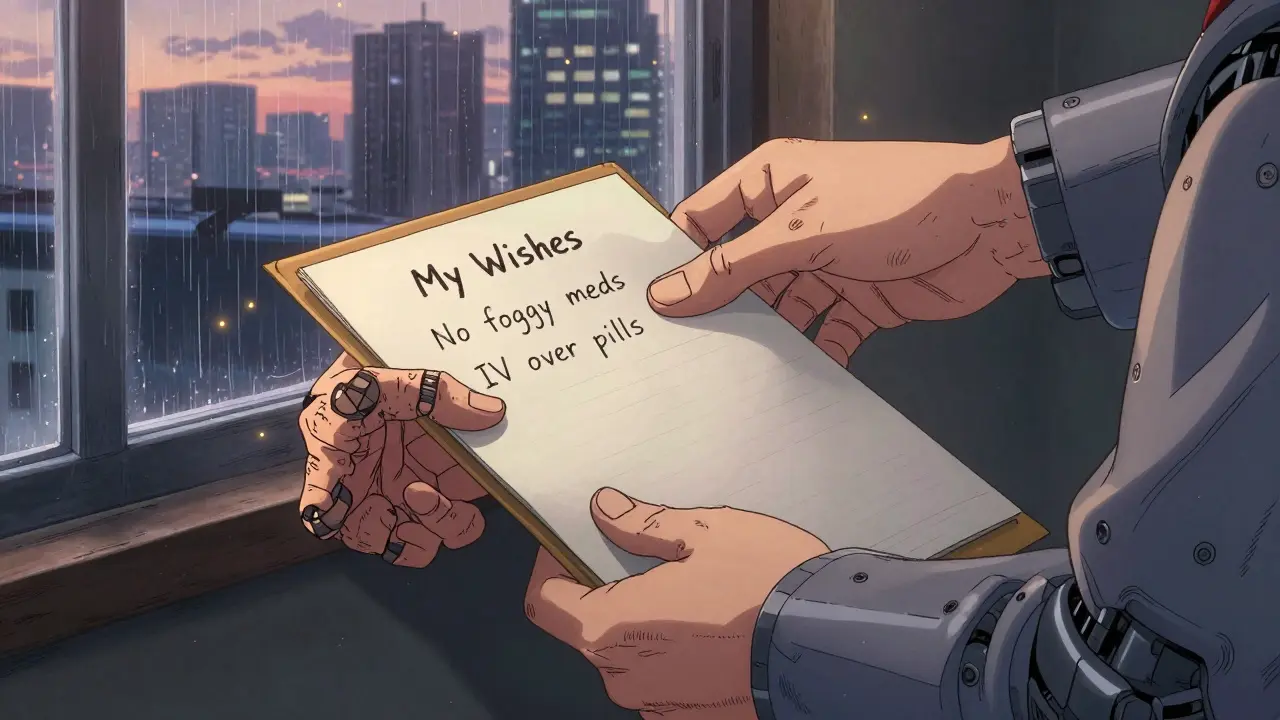
- “I hate feeling foggy. If I’m on a lot of pain meds that make me drowsy, I’d rather be uncomfortable than confused.”
- “I’d rather take a pill than get a shot if I can. But if I’m too sick to swallow, I’m okay with an IV.”
- “If I have dementia and I’m screaming because I’m scared, I don’t want to be sedated unless it’s the only way to keep me safe.”
- “I don’t want antibiotics if I’m near the end and they’re just buying time.”
Use real examples. Talk about your grandparent’s experience. Mention a movie or news story that stuck with you. Ask your agent: “What would you do if you were me?”
Write these down. Not in legalese. Just in your own words. Give the list to your agent. Keep a copy with your medical records.
What About POLST and Other Forms?
POLST (Physician Orders for Life-Sustaining Treatment) is different. It’s not a proxy. It’s a medical order - signed by your doctor - that tells EMS and hospitals exactly what to do. It’s for people with serious, advanced illness. It covers things like: “Do not resuscitate,” “No IV antibiotics,” “No feeding tube.”It’s not a replacement for a Medical Power of Attorney. It’s a companion. If you’re healthy, get the proxy. If you’re in hospice or have a terminal diagnosis, get both.
By December 2025, Medicare and Medicaid facilities will be required to store POLST forms in electronic records. That means your wishes could be visible to every doctor who treats you - if you’ve filled one out.

What Happens If You Don’t Have One?
If you don’t name an agent, the law steps in. In most states, it’s your spouse, then adult children, then parents. But what if you’re not married? What if your kids fight? What if your mom thinks you’d want everything done - but your brother knows you’d refuse?That’s when courts get involved. That’s when you get the wrong meds. That’s when your family spends weeks in conflict instead of being together.
And it’s not rare. Only 36.7% of U.S. adults have any advance directive. Among people under 45? Just 24.8%. That means more than 75% of younger adults have no plan. No voice. No backup.
How to Get Started - Right Now
You don’t need a lawyer. You don’t need to wait until you’re sick.Here’s your 10-minute plan:
- Choose your agent. Talk to them. Make sure they say yes.
- Have the conversation. Write down your medication preferences in plain language.
- Download your state’s free Medical Power of Attorney form from LawHelp DC or your state health department.
- Fill it out. Sign it. Get the required witnesses or notary.
- Give copies to your agent, your doctor, and your family. Keep one in your wallet or phone.
- Review it every year - or after any big change (new diagnosis, divorce, move).
There are free apps like PREPARE (from UCSF) that walk you through video scenarios to help you think through your choices. They’re not magic. But they help you say what you mean.
The Real Reason This Matters
This isn’t about legal paperwork. It’s about dignity. It’s about control. It’s about making sure the last thing someone hears isn’t a doctor asking, “What do you want us to do?” - while you’re too weak to answer.It’s about knowing that when your time comes, someone you trust will stand up for you - not just with machines, but with pills, with pain relief, with quiet dignity.
You don’t have to be old. You don’t have to be sick. You just have to care - enough to speak up before you can’t.
Can my agent refuse medication even if the doctor says it’s necessary?
Yes - if your agent knows your wishes and the medication goes against them. Doctors must follow your agent’s decisions as long as they’re based on your stated preferences. But if the agent’s decision violates state law (like refusing life-saving treatment for a minor), the hospital can challenge it in court.
Do I need a lawyer to create a Medical Power of Attorney?
No. All 50 states offer free, state-specific forms online. You just need to sign it correctly - usually with two witnesses or a notary. A lawyer is only helpful if you have complex medical conditions, multiple marriages, or family conflict.
Can I change my agent later?
Yes. You can revoke or change your Medical Power of Attorney anytime as long as you’re mentally capable. Just fill out a new form, destroy the old one, and tell everyone involved.
What if my family disagrees with my agent’s decision?
Legally, your agent has the final say - as long as they’re following your known wishes. But family conflict is common. The best protection is having clear, documented conversations ahead of time. If your agent is acting in bad faith, others can go to court - but that’s rare and takes time.
Does this cover mental health and psychiatric medications?
In most states, yes - but some, like Indiana, require a separate psychiatric advance directive with a doctor’s signature. Make sure your agent knows your views on sedatives, antipsychotics, or forced treatment. These are often the most emotionally charged decisions.
Are digital advance directives reliable?
Yes - if they’re legally valid in your state. Apps like PREPARE help you clarify your wishes, but you still need to sign a paper form for it to be legally binding. Digital storage (like DocuBank or Everplans) helps ensure your documents are accessible in emergencies, especially if your phone or cloud account is linked to your medical records.